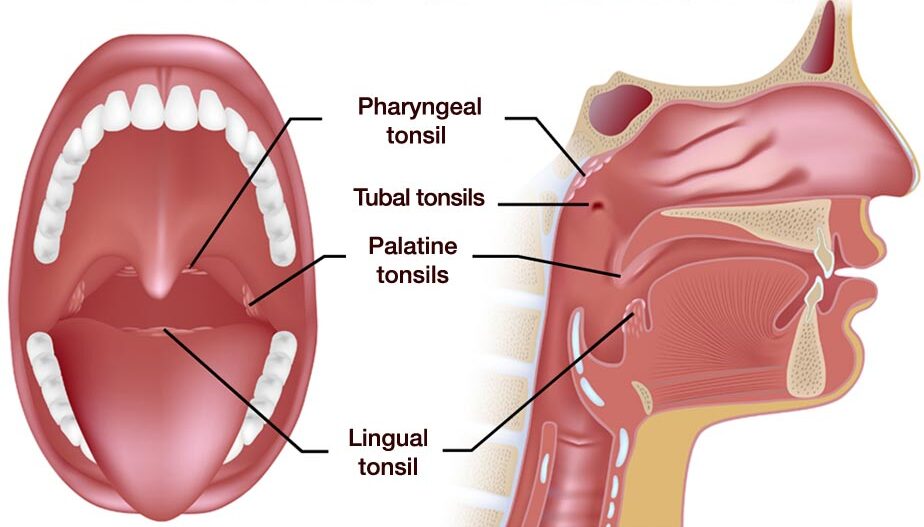
Tonsillitis is an infection of tonsils, which are two masses of tissue at the back of throat.
Tonsils act as filters, trapping germs that could otherwise enter your airways and cause infection. They also make antibodies to fight infection. But sometimes, they get overwhelmed by bacteria or viruses. This can make them swollen and inflamed.
Tonsillitis is common, especially in children. It can happen once in a while or come back again and again in a short period.
There are three types:
1. Acute Tonsillitis. These symptoms usually last 3-4 days but can persist for up to 2 weeks.
2. Recurrent Tonsillitis. This is when tonsillitis occurs several times a year.
3. Chronic Tonsillitis. A long-term tonsil infection.
Symptoms
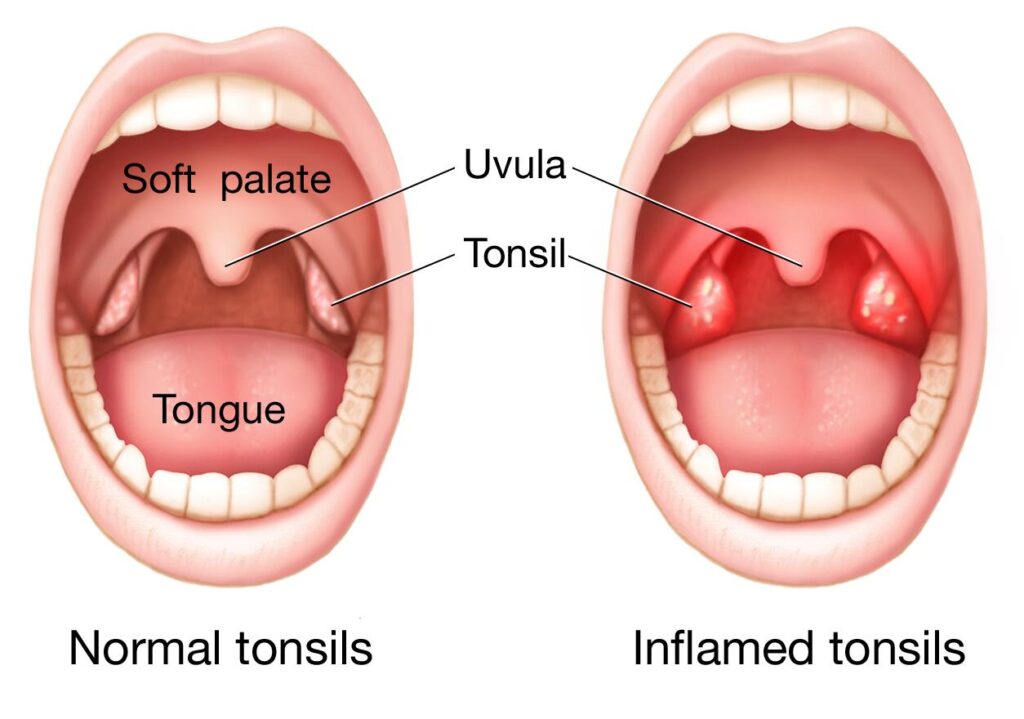
The main symptoms of tonsillitis are inflamed and swollen tonsils, sometimes severe enough to make it hard to breathe through mouth. Other symptoms include:
- Throat pain or tenderness
- Fever
- Red tonsils
- A white or yellow coating on your tonsils
- Painful blisters or ulcers on your throat
- Headache
- Loss of appetite
- Ear pain
- Trouble swallowing
- Swollen glands in your neck or jaw
- Fever and chills
- Bad breath
- A scratchy or muffled voice
- Stiff neck
Symptoms in Children
In children, tonsillitis symptoms may also include:
- Upset stomach
- Vomiting
- Stomach pain
- Drooling
- Not wanting to eat or swallow
Causes of Tonsillitis
Both bacterial and viral infections cause tonsillitis. It is important to determine the correct cause in order to find the right treatment.
Viral Tonsillitis
Several different viruses may make tonsils inflamed, leading to tonsillitis. Some include:
- Adenoviruses
- Influenza virus
- Epstein-Barr virus
- Parainfluenza viruses
- Enteroviruses
- Herpes simplex virus
- HIV
Generally, viral tonsillitis is less severe and more common than bacterial tonsillitis, making up about 70% of cases.
Bacterial Tonsillitis
Another common cause of tonsillitis is Streptococcus (strep) bacteria, which can also lead to strep throat. Occasionally other bacteria, such as Staphylococcus aureus, can inflame tonsils as well.
Bacterial tonsillitis sometimes leads to a condition called quinsy. This occurs when an abscess (or a buildup of pus) develops next to tonsil, pushing it toward the center of throat. Quinsy can be quite painful, and can even make it difficult to open your mouth.
The first signs of tonsillitis
A sore throat is often the first symptom of tonsillitis. If you develop a sudden sore throat, keep an eye on tonsils to see if they get red or swollen.
How does tonsillitis spread?
The viruses and bacteria that cause tonsillitis are highly contagious. They’re passed along by:
- Sharing utensils, foods or drinks.
- Coming into close contact with someone who’s sick.
- Touching a contaminated surface and then touching your nose or mouth.
- Inhaling tiny particles that become airborne when a sick person sneezes or coughs.
Risk factors
You have an increased risk of getting tonsillitis if you’re:
- Between the ages of 5 and 15. Tonsillitis is most common in children and adolescents.
- Exposed to germs frequently. Those who work or go to school in buildings with lots of other people have a higher risk of encountering the germs that cause tonsillitis.
Diagnosis
Doctor will start with a physical exam that will include:
- Using a lighted instrument to look at your child's throat and likely his or her ears and nose, which also may be sites of infection
- Checking for a rash known as scarlatina, which is associated with some cases of strep throat
- Gently feeling (palpating) your child's neck to check for swollen glands (lymph nodes)
- Listening to his or her breathing with a stethoscope
- Checking for enlargement of the spleen (for consideration of mononucleosis, which also inflames the tonsils)
Throat swab
With this simple test, a sterile swab rubbed over the back of your child's throat to get a sample of secretions. The sample will be checked in the clinic or in a lab for streptococcal bacteria.
Complete blood cell count (CBC)
Doctor may order a complete blood cell count (CBC) with a small sample of child's blood. The profile of what's elevated, what's normal or what's below normal can indicate whether an infection is more likely caused by a bacterial or viral agent. A CBC is not often needed to diagnose strep throat. However, if the strep throat lab test is negative, the CBC may be needed to help determine the cause of tonsillitis.
Conventional Treatment
Treatment for tonsillitis typically involves managing pain with analgesics and ensuring adequate oral hydration. Symptomatic relief can be achieved with medications like steroids and NSAIDs. Streptococcus pyogenes is the most common bacterial cause of tonsillitis, and the preferred antibiotics are penicillins, administered either as a 10-day oral course or a single injection of benzathine penicillin G into the muscle. For patients allergic to penicillin, alternatives include a 5-day course of azithromycin or a 10-day course of cephalosporin or clindamycin. These treatments aim to address the bacterial infection effectively while managing symptoms to promote recovery.
Complications
While tonsillitis is typically symptomatically managed with good clinical outcomes, complications do occur. Abscesses, rheumatic fever, scarlet fever, and acute glomerulo-nephritis are known complications.
Homoeopathic Approach
Tonsillitis can be effectively treated without resorting to surgery through homeopathic remedies. Homeopathic treatment for tonsillitis focuses on prescribing medicines based on the complete set of symptoms a patient presents, which includes mental, physical, familial, historical, and social aspects. By addressing this totality of symptoms, a unique medicine is selected for each patient. These medicines aim to strengthen the patient's immune system, correcting any weaknesses that make them susceptible to viral infections. Homeopathic medicines are known for being free of side effects, allowing patients to use them for extended periods without complications. They are safe for all age groups, including pregnant women.
Facts
- Tonsils and adenoids are considered as the first line of defense against infection entering through the mouth and nose.
- Removal of the tonsils / adenoids may resolve immediate discomfort. However your susceptibility to catch colds and throat infections does not reduce.
- A poor immune response to allergens, viruses and infection may continue to exist even after surgery. One may suffer from repeated pharyngitis (sore throat) and may be prone to allergens.
- Ideally, saving the tonsils/adenoids and improving your immune response to future infections will guarantee a superior prognosis.
- Research shows that removal of tonsils and adenoids does not impact future immunity. However, the reason for repeated attacks is poor immunity. Therefore, improving this immune response is crucial in saving the tonsils / adenoids. If the immune response is boosted there would be no need for their removal.
- Specialized homeopathic treatments based on an individual’s signs and symptoms does help in boosting immune responses, lowering recurrent infection and susceptibility to allergens, as well as preventing surgery in most cases.